$629 Band-Aids and $20,243 Bike Crashes: The High Prices of America’s Emergency Rooms
What policy options and consumer tactics can reduce “surprise billing” for emergency room visits?


Register
Course Information
- Audience: Public health workforce interested in high cost of emergency room visits
- Format: Recorded Webinar
- Date/Time: Wednesday, February 10, 2021 1:00 PM - 2:30 PM
- Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hour. Maximum advanced-level continuing education contact hour is 1. Provider ID: 1131137 Event ID: SS1131137_HPAER.
If you are not seeking a CHES/MCHES contact hours, If you complete the evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course. - Competencies: Policy Development and Program Planning Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials: None
- Pre-requisites: None
About this Recording
Americans make more than 140 million trips to the emergency room each year, but usually don’t know the price until a bill shows up in the mail. New York Times journalist Sarah Kliff spent 18 months collecting thousands of emergency room bills, and made public the prices that hospitals try to keep secret. From $629 Band Aids to $5,571 charges for just sitting in a waiting room, Ms. Kliff will discuss what her reporting found, what it tells us about the American health care system, and the policy solutions Congress could use to fix it.
What you'll learn
At the end of the recording, participants will be able to:
- Describe legislative and policy relief for “surprise billing” to patients
- List 3 loop-holes in the “No Surprises Act”
- Describe tactics patients can use to advocate for themselves in terms of hospital billing
- Discuss relative benefit of various policy options (e.g., patient choice, increase in transparency, rate-setting) in reducing hospital costs
Moderator

Wendy Mariner
Emeritus Professor, BU School of Public Health
Professor Mariner is the Edward R. Utley Professor of Health Law at Boston University School of Public Health, Professor in the Center for Health Law, Ethics & Human Rights, Professor in the Department of Health Law, Policy & Management, and Director of the JD-MPH dual degree program at Boston University School of Public Health; Professor of Law at Boston University School of Law; and Professor of Medicine at Boston University School of Medicine. Professor Mariner’s research focuses on laws governing health risks, including social and personal responsibility for risk creation, health insurance systems, implementation of the Affordable Care Act, ERISA, health information privacy, and population health policy. She has co-authored three editions of the law school textbook, PUBLIC HEALTH LAW, Third Edition (Wendy Mariner, George J Annas, Nicole Huberfeld & Michael Ulrich, 2019), Second Edition (Wendy Mariner & George J Annas, 2014), and First Edition (Ken Wing, Wendy Mariner, George Annas & Dan Strouse, 2007), and published more than 100 articles in the legal, medical and health policy literature on public health law, patients and consumers’ rights, health care reform, insurance benefits and regulation, AIDS policy, immunization, research with human beings, and reproductive rights. She is Chair of the American Bar Association Section of Civil Rights and Social Justice, having previously served as Vice Chair and Secretary, and was a member of the ABA Special Committee on Bioethics and the Law. Professor Mariner also serves as Program Chair of the Program in Health Law & Human Rights, a joint project with the Public Health Regulations Analysis Center of the National School of Public Health of the New University of Lisbon. Professor Mariner has served on state, national, and international boards and commissions, including the Massachusetts Health Facilities Appeals Board, the Massachusetts Health Care Quality and Cost Council Advisory Committee, the Massachusetts Health Information Technology Council Advisory Committee; the National Institutes of Health AIDS Advisory Committee, the Committee for the International Ethical Guidelines for Biomedical Research Involving Human Subjects, the Executive Board of the American Public Health Association, and Institute of Medicine committees. Her university activities have included serving as Chair of the Boston University Faculty Council and ex officio member of the Trustees of Boston University, Co-Director of Regulatory Knowledge and Research Ethics of Boston University’s Clinical and Translational Science Institute, and member of the Boston University Task Force on Diversity and Inclusion and other university committees. She was the American Journal of Public Health’s Contributing Editor for Health Law and Ethics and currently serves on the editorial boards of Journal of Health Politics, Policy & Law, the Journal of Law, Medicine & Ethics, and the Human Rights and the Global Economy. With health law colleagues, she has submitted amicus curiae briefs to the Supreme Court of the United States in cases involving health law issues, including the constitutionality of the Affordable Care Act.
Subject Matter Expert

Sarah Kliff
Investigative Reporter, The New York Times
Sarah Kliff is one of the country’s leading health policy journalists, who has spent nearly a decade chronicling Washington’s battle over the Affordable Care Act. Her reporting has inspired new legislation in Congress, been cited by the Supreme Court, and resulted in multiple hospitals revising their billing policies.
Sarah is currently an investigative reporter at the New York Times and, before that, was a senior policy correspondent at the website Vox. She has also covered health care for the Washington Post, Politico, and Newsweek magazine.
Sarah is the recipient of multiple reporting awards, including fellowships from the Association of Health Care Journalists and the Annenberg School of Journalism at the University of Southern California. The Supreme Court cited Sarah’s work in their 2012 decision upholding the health care law. After she broke news in early 2017 that Republican legislators had exempted their own coverage from their Obamacare repeal bill, the House of Representatives took a vote to close that loophole.
Sarah is a frequent television guest and has appeared on CBS, PBS, Fox News, CNN, and MSNBC. She enjoys public speaking and, most recently, has presented at the Harvard Kennedy School of Government, the Aspen Ideas Festival, the Colorado Health Institute and the California Health Care Foundation.
Registration and Contact Hours
Select the Enroll button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
* Yale School of Public Health, Office of Public Health Practice, a New England Public Health Training Center partner, is a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. All CHES credit inquiries are managed by YSPH

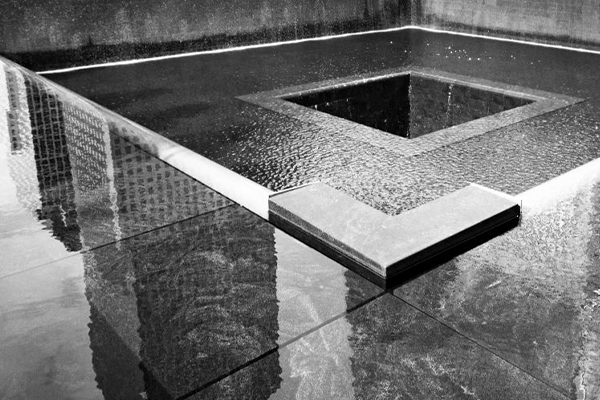
9/11. Twenty Years Later
Do you remember where you were on 9/11/2001? That’s the date of multiple terrorist attacks in the United States that killed and wounded thousands of people and continue to impact population health, both mental and physical.


Register
Course Information
- Audience: Public Health Professionals
- Format: Webinar
- Date/Time: Friday, September 10th 10:00 AM – 11:30 AM EST
- Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 1. Provider ID: 1131137 Event ID: SS1131137_911TYL.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Public Health Sciences Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
This year commemorates the 20th Anniversary of 9/11. To mark this date, we are hosting a conversation about the events of September 11th and the health of the public. Our panelists will reflect on what we learned about health post-9/11, and what implications this event had for population health science today.
What you'll learn
At the end of the recording, participants will be able to:
- List key long-term health findings from the World Trade Center (WTC) Health Registry
- Explain innovations in the treatment of post-traumatic stress disease (PTSD)
- Describe implications for future disaster preparedness efforts based on research findings from the WTC Health Program
- State a recommendation about mental health treatment based on findings from the Mount Sinai research on mothers who were at the WTC when the towers collapsed and suffered from PTSD
- Give examples of how systematic racism and classism influenced the population health impacts of 9/11
Subject Matter Experts

Barbara Rothbaum
@EMORYMEDICINE
Professor in Psychiatry, Director of Emory Healthcare Veterans Program, Emory School of Medicine
Barbara Olasov Rothbaum, PhD is Director of the Emory Healthcare Veterans Program. She is a professor and Associate Vice Chair of Clinical Research at Emory School of Medicine in the Department of Psychiatry and Behavioral Sciences and Director of the Trauma and Anxiety Recovery Program and holds the Paul A. Janssen Chair in Neuropsychopharmcology. Dr. Rothbaum specializes in research on the treatment of anxiety disorders, particularly PTSD. She was a member of the Institute of Medicine’s (IOM) Study on Assessment of Ongoing Efforts in the Treatment of PTSD, and briefed the DOD, VA, House and Senate Committees on Veterans Affairs and Armed Services Committees on the IOM report results. Dr. Rothbaum has been studying PTSD treatments since 1986 and has developed, tested, and disseminated some of the most innovative and effective treatments available for PTSD. She is an inventor of virtual reality exposure therapy. She was a pioneer in applying it in the treatment of PTSD in combat veterans. She has authored over 400 scientific papers and chapters, has published 11 books on the treatment of PTSD and edited 4 others on anxiety, and received the Diplomate in Behavioral Psychology from the American Board of Professional Psychology. She is a past president of the International Society of Traumatic Stress Studies (ISTSS), is currently on the Scientific Advisory Boards for the Anxiety Disorders Association of America (ADAA), National Center for PTSD (NC-PTSD), and the executive committee of the Warrior Care Network. She is a fellow of the ACNP (American College of Neuropsychopharmacology), the National Academy of Inventors (NAI), the Association for Behavioral and Cognitive Therapies (ABCT), and American Psychological Association’s Division 56 (Division of Trauma Psychology) and was awarded the 2010 “Award for Outstanding Contributions to the Practice of Trauma Psychology” for APA Division 56 and the Robert S. Laufer Award for Outstanding Scientific Achievement from the International Society for Traumatic Stress Studies (ISTSS).

David Vlahov
@DAVID_VLAHOV
MODERATOR, Associate Dean for Research and Professor, Yale School of Nursing, and Professor of Epidemiology, Yale School of Public Health
David Vlahov is associate dean for research and professor at the Yale School of Nursing and a professor of epidemiology at the Yale School of Public Health. His primary area of focus has been on urban health. His studies in Baltimore, Harlem, and the Bronx, which have served as a platform for subsequent individual, community, and policy intervention studies. This work has contributed new knowledge to promote health equity. Vlahov was the founding president of the International Society for Urban Health. He has been a visiting professor at the medical school in Belo Horizonte, Brazil, and served as an expert consultant to the World Health Organization’s Urban Health Center in Kobe, Japan. Vlahov is the editor-in-chief of the Journal of Urban Health, has edited three books on urban health, and has published over 654 scholarly papers. He was the principal investigator of the Rockefeller Foundation project on the Roundtable for Urban Living Environment Research on urban health metrics and a member of the WHO Knowledge Network for Urban Settlements as part of the WHO Commission on the Social Determinants of Health. Vlahov served on the New York City Board of Health, and is a member of the National Academy of Medicine currently serving on the institute’s Board of Global Health.

Albeliz Santiago Colon
@WTCHEALTHPRGMAssociate Service Fellow, World Trade Center Health Program,
Research Planning & Care Integration UnitAlbeliz Santiago-Colón, Ph.D., is an Associate Service Fellow in the Research Planning & Care Integration Unit at the World Trade Center (WTC) Health Program, which is administered by the National Institute for Occupational Safety and Health (NIOSH), under the Centers for Disease Control and Prevention. The Program provides no-cost medical monitoring and treatment for certified WTC-related health conditions to those directly affected by the 9/11 attacks in New York, the Pentagon, and in Shanksville, Pennsylvania. Dr. Santiago-Colón assists with integrating research findings of the health impacts arising from the 9/11 attacks into the care and well-being of members. She recently coauthored a review article “World Trade Center Health Program: First Decade of Research” where she compiled and analyzed over two decades worth of research to support translational research. Within the Health Program, she specializes in uncovering knowledge gaps to inform future research needs. Before joining the WTC Health Program in 2019, she was an Oak Ridge Institute for Science and Education (ORISE) fellow at the Division of Field Studies and Engineering under NIOSH. While working as an ORISE fellow, she completed her dissertation on the association between maternal occupational exposure to polycyclic aromatic hydrocarbons and selected birth defects of the face and central nervous system using data from the National Birth Defects Prevention Study. Originally from Puerto Rico, she received a B.S. in Biology from the University of Puerto Rico and a Ph.D. in Epidemiology from the University of Cincinnati. Her training in epidemiology has focused on environmental health, maternal and child health, and occupational exposure assessment.

Rachel Yehuda
@RACHELYEHUDA
Professor and Vice Chair of Psychiatry, Icahn School of Medicine at Mount Sinai
Rachel Yehuda, Ph.D. is a Professor and Vice Chair of Psychiatry, and Professor of Neuroscience at the Icahn School of Medicine at Mount Sinai. She is also the Mental Health Director at the Bronx Veterans Affairs. Dr. Yehuda is a recognized leader in the field of traumatic stress studies and has authored hundreds of papers and 10 books in the field of traumatic stress and the neuroscience of PTSD. She is the recipient of numerous awards and federal grants. Her current interests include PTSD prevention and innovative approaches to treatment, the study of risk and resilience, epigenetics and the intergenerational transmission of trauma and PTSD. She is a member of the National Academy of Medicine and has recently established a Center for Psychedelic Psychotherapy and Trauma Research at Mount Sinai.

Mark Farfel
@NYCHEALTHY
Director,
World Trade
Center Health Registry
New York City Department of Health
and Mental Hygiene
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.

Abolition, Incarceration, and the Public’s Health
Recently, the issue of prison reform has been gaining national attention, forcing policymakers to rethink the issue. As momentum grows to call for change, how does public health play a role in ending mass incarceration and reforming a criminal justice system?


Register
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Wednesday, September 28, 2022, 1:00 PM – 2:30 PM ET
- Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1.5 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_09282022If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Policy Development and Program Planning Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
The United States is the most incarcerated nation in the world. Decades of harmful policies have led to overcrowded prisons and a broken criminal justice system, leading to prison populations that are disproportionately poor and people of color. Recently, the issue of prison reform has been gaining national attention, forcing policymakers to rethink the issue. As momentum grows to call for change, how does public health play a role in ending mass incarceration and reforming a criminal justice system?
What you'll learn
At the end of the recording, participants will be able to:
- Explain how housing can be a point of intervention to reduce the risk of incarceration
- Describe the abolitionist approach to end cycles of incarceration
- Compare community violence intervention and alternative community first responder programs to the criminal justice system approach currently in place in the United States
- Give examples of courses that can train public health students to understand and develop strategies to address mass criminalization and mass incarceration
- Discuss how an integrated advocacy approach, using public health research, can support abolishment of major systems of oppression
Moderator

Deborah Douglas
@DEBOFFICIALLYCo-Editor in Chief, The Emancipator

Angela Aidala
@COLUMBIAMSPH
Associate Research Scientist, Columbia Mailman School of Public Health
Dana Rice
@DKRICEDRPH
Assistant Professor, University of North Carolina Gillings School of Global Public Health
Insha Rahman
@VERAINSTITUTE
Vice President of Vera Action, Vice President of Advocacy and Partnerships
Emile DeWeaver
@PRSNRENAISSANCE
Author; Co-founder,
Prison Renaissance
Zal Shroff
@LCCRSF
Senior Attorney, Racial Justice, Lawyers' Committee for Civil Rights
DEBORAH D. DOUGLAS is co-editor in chief of The Emancipator. She previously served as the Eugene S. Pulliam Distinguished Visiting Professor at DePauw University, senior leader with The OpEd Project, amplifying underrepresented expert voices, and founding managing editor of MLK50: Justice Through Journalism. While teaching at Northwestern University, she spearheaded a graduate investigative journalism capstone on the Civil Rights Act of 1964 and taught best practices in Karachi, Pakistan. Douglas’ adventures in thought leadership were seeded at the Chicago Sun-Times where she served as Deputy Editorial Page Editor/Columnist. Deborah is author of the “U.S. Civil Rights Trail: A Traveler’s Guide to the People, Places, and Events That Made the Movement” (Moon, 2021), the first-ever travel guide to follow the official civil rights trail in the South, and a contributor to “Four Hundred Souls: A Community History of African America, 1619-2019” (OneWorld, 2021). Among her many recognitions, she received Chicago’s prestigious Studs Terkel Award and the Society of American Travel Writers 2021 Guidebook of the Year.
Subject Matter Experts
Angela A. Aidala, Ph.D., is a Research Scientist at the Columbia University Mailman School of Public Health in the Department of Sociomedical Sciences. Her major interest is research, teaching, and service delivery strategies to work effectively with harder to reach or ‘hidden’ populations in urban settings crucial to understanding health disparities: disadvantaged and socially marginalized youth and adults challenged by unstable housing/ homeless experience, mental illness, substance use, and/or criminal justice involvement. She is committed to applied research — working with community members, policy makers, service providers, and advocates to translate research to inform policy and program decision making. Dr. Aidala currently leads a 10 year follow-up of a demonstration project that brought together multiple governmental agencies (Corrections, Homeless Services, Health), housing providers, and community stakeholders for a housing-based intervention for adults with complex needs and histories of cycling in and out of incarceration, homelessness, and crisis health care institutions – the Frequent Users Services Engagement (FUSE) initiative. Documented success of the original project has inspired multiple jurisdictions throughout the US to launch similar efforts. The FUSE long term follow-up study analyzes the role of stable housing as a critical component of successful community reentry, not just in the short term but considering impacts over the life course. We examine longitudinal trajectories among multiple life domains –incarceration, housing, and health – analyzing interdependencies and policy and institutional contexts.
Dana Rice, DrPH, assistant professor, is a public health practitioner and researcher who examines best practices in public health leadership and community engagement with a health equity, social justice and human rights lens. Her primary focus is on the integration of public health and correctional health systems and the impact of mass criminalization and mass incarceration on public health. She was a recipient of the student-nominated Award for Excellence in Teaching and Innovation, the peer-nominated Delta Omega Faculty Award and a UNC Equity in Teaching fellow. Prior to joining the faculty at Gillings, Dr. Rice spent 20 years working in the public, private and non-profit sectors. Her most recent work was dedicated to designing, implementing and evaluating an HIV/STD screening program in a large urban jail and training graduate public health and medical students in translating applied public health practice skills to a variety of community settings.
Insha Rahman is Vice President for Advocacy and Partnerships at the Vera Institute of Justice and Vice President of Vera Action, Vera’s 501c4 sister organization. She leads the development of Vera and Vera Action’s advocacy priorities and campaigns across the organization, partnering with government, advocates, and organizers to win policy change to end mass incarceration and build safe, thriving communities for all. Insha is a nationally recognized expert on bail reform and pretrial justice. In addition to overseeing Vera and Vera Action’s advocacy priorities, she supervises the organization’s place-based initiatives in California, Louisiana, and New York. She has been quoted as an expert in several outlets, including The New York Times, NPR, and PBS. Prior to joining Vera, she was a public defender at The Bronx Defenders. She graduated with a BA in Africana Studies from Vassar College and earned her J.D. from the City University of New York School of Law.
Emile is an African-American activist whose life sentence in prison was commuted by California’s Governor Brown after 21 years for his community work in prison. While in prison, he was a culture writer for Easy Street Magazine; he co-founded Prison Renaissance, and despite the criminalization of organizing in California prisons, he covertly organized in prison to pass legislation that changed the way California treats juveniles in its criminal legal system. Currently Emile holds workshops on abolitionist strategies to develop policy and programs, and he’s working on his memoir for The New Press titled Ghost in the Prison Industrial Machine.
Zal is a Senior Staff Attorney on the Racial Justice team. Prior to joining LCCRSF, Zal was a Clinical Lecturer-in-Law at Yale Law School where he worked with students to improve ballot access for incarcerated individuals and supervised litigation against the federal Bureau of Prisons for its response to the pandemic. Before that, Zal was a Staff Attorney at the ACLU of Kansas where he worked on a variety of civil rights cases spanning conditions of confinement, prosecutorial/police accountability, voting rights, race and religious discrimination, and First Amendment issues. Immediately after law school, Zal was the Clifford Chance Foundation Fellow at the Vera Institute of Justice, where he worked on non-profit in-house regulatory and compliance matters, and spearheaded a project on accessing state financial aid dollars for college in prison programs nationwide. Zal is a graduate of Brown University and received his JD from Columbia Law School. He is admitted to practice in New York, Connecticut, and Kansas, and is an MJP Registered Legal Aid Attorney in the State of California.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of award 2 UB6HP31685‐05‐00 “Public Health Training Centers.” The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government.

Annual Shine Lecture: Sheri Fink - Patient Rights in Emergencies: The Right to Treatment and the Right to Refuse Treatment.
Who should be part of the decision-making process for medical care allocation in an emergency? What is the appropriate role for the patients themselves? Who gets to make the final decision?


Register
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Wednesday, April 13th, 2022 1:00 PM – 2:00 PM EST
- Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_ASLPRE.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Public Health Sciences Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
Boston University School of Public Health’s Center for Health Law, Ethics & Human Rights presents the annual Cathy Shine lecture. The lectureship honors the memory of Cathy Shine and her dedication to the rights of all those in need of care. This year’s event will feature author and filmmaker Sherri Fink. Her best-selling book Five Days at Memorial: Life and Death in a Storm-Ravaged Hospital focused on the tough choices made in the aftermath of Hurricane Katrina. She is also the co-creator and executive producer of the Emmy-nominated documentary series Pandemic: How to Prevent an Outbreak.
What you'll learn
At the end of the recording, participants will be able to:
- Describe common challenges to medical ethics and health equity
- Discuss ethical framework for how to prioritize allocation of medical care in a crisis
- Discuss the elements of a just decision-making process
- Assess lessons learned from experience in 3 real-life cases (Hurricane Katrina, Superstorm Sandy, COVID-19)
Moderator

George Annas
@GEORGEJANNAS
William Fairfield Warren Distinguished Professor of Health Law, Ethics & Human Rights, Boston University School of Public Health
Sheri Fink
@SHERIFINK
Author, Five Days at Memorial: Life and Death in a Storm-Ravaged Hospital
George J. Annas is William Fairfield Warren Distinguished Professor at Boston University and Director of the Center for Health Law, Ethics & Human Rights at Boston University School of Public Health, and a member of the Department of Health Law, Policy and Management at the School of Public Health. He is also a Professor at the School of Law and School of Medicine. He is author or editor of 20 books on health law and bioethics, including The Rights of Patients (3d ed 2004), Public Health Law (2d ed 2014), American Bioethics (2005), Worst Case Bioethics (2010), and Genomic Messages (2015). He is a member of the National Academy of Medicine and a Fellow of the American Association for the Advancement of Science. He is the co-founder of Global Lawyers & Physicians, a NGO dedicated to promoting health and human rights.
Subject Matter Expert
Sheri Fink is the author of the New York Times bestselling book Five Days at Memorial: Life and Death in a Storm-Ravaged Hospital about choices made in the aftermath of Hurricane Katrina. She is a co-creator and an executive producer of the Emmy-nominated Netflix documentary television series Pandemic: How to Prevent an Outbreak (2020), filmed the year prior to the Covid-19 pandemic. Fink contributed to the New York Times’ Pulitzer Prize-winning coverage of the pandemic. Her and her colleagues’ stories on Ebola in West Africa were recognized with the 2015 Pulitzer Prize for international reporting, the George Polk Award for health reporting, and the Overseas Press Club Hal Boyle Award. Her story “The Deadly Choices at Memorial,” co-published by ProPublica and the New York Times Magazine, received a 2010 Pulitzer Prize for investigative reporting and a National Magazine Award for reporting. Fink is an adjunct associate professor at the Tulane School of Public Health and Tropical Medicine. A former relief worker in disaster and conflict zones, she received her M.D. and Ph.D. from Stanford University. Her first book, War Hospital: A True Story of Surgery and Survival (PublicAffairs), is about medical professionals under siege during the genocide in Srebrenica, Bosnia-Herzegovina. Five Days at Memorial was the winner of the National Book Critics Circle Award for nonfiction, the PEN/John Kenneth Galbraith Award for nonfiction, the Ridenhour Book Prize, the J. Anthony Lukas Book Prize, the Los Angeles Times Book Prize, the Southern Independent Booksellers Alliance Book Award, the American Medical Writers Association Medical Book Award, and the NASW Science in Society Journalism Book Award.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Tuesday, April 4, 2023, 1:00 PM – 2:00 PM ET
- Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_ASLTCPHCA.If you are not seeking CHES/MCHES contact hours, if you complete the evaluations, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Public Health Sciences Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
Boston
University School of Public Health’s Center for Health Law, Ethics & Human
Rights presents the annual Cathy Shine lecture. The lectureship honors the
memory of Cathy Shine and her dedication to the rights of all those in need of
care. This year’s event will feature Dr. Heidi B. Kummer (SPH ’04). Dr. Kummer
is the founder of the independent practice 3C Patient Advocacy and has served as
President of the Patient Advocate Certification Board since 2021.
What you'll learn
At the end of the recording, participants will be able to:
- Describe who health care advocates are and what they do
- Discuss the benefits of certification for patient and health care advocacy professionals
- Discuss what the pandemic taught us about patient safety and shared decision making
- Recognize the challenges we are still facing regarding patient rights advocacy
Moderator

George Annas
William Fairfield Warren Distinguished Professor, Boston University; Director of the Center for Health Law, Ethics & Human Rights, Boston University School of Public Health

Heidi B. Kummer
President, Patient Advocate Certification Board (SPH '04)
Dr. Zaman is a Howard Hughes Medical Institute Professor of Biomedical Engineering and Global Health at Boston University. He also serves as the Director of Boston University’s Center on Forced Displacement. He received his master’s and P.h.D from the University of Chicago. In addition to five books and over 130 peer-reviewed research articles, Professor Zaman has written extensively on innovation, refugee and global health in newspapers around the world. His newspaper columns have appeared in over 30 countries and have been translated into eight languages. He has won numerous awards for his teaching and research, the most recent being Guggenheim Fellowship (2020) for his work on antibiotic resistance in refugee camps.
Subject Matter Expert
George J. Annas is William Fairfield Warren Distinguished Professor at Boston University and Director of the Center for Health Law, Ethics & Human Rights at Boston University School of Public Health, and a member of the Department of Health Law, Policy and Management at the School of Public Health. He is also a Professor at the School of Law and School of Medicine. He is author or editor of 20 books on health law and bioethics, including The Rights of Patients (3d ed 2004), Public Health Law (2d ed 2014), American Bioethics (2005), Worst Case Bioethics (2010), and Genomic Messages (2015). He is a member of the National Academy of Medicine and a Fellow of the American Association for the Advancement of Science. He is the co-founder of Global Lawyers & Physicians, a NGO dedicated to promoting health and human rights.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of award 2 UB6HP31685‐05‐00 “Public Health Training Centers.” The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government.

Course Information
- Audience: Public Health Professionals
- Format: Webinar
- Date/Time: Monday, April 5th 2021, 4:30 PM – 6 PM EST.
- Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 1. Provider ID: 1131137 Event ID: SS1131137_AHP1.
If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course. - Competencies: Data Analytics and Assessment Skills
- Learning Level: Awareness
- Companion Trainings: Antiracism as Health Policy (Part 2)
Antiracism as Health Policy (Part 3) - Supplemental materials:None
- Pre-requisites: None
About this Recording
Part 1: Data, race, and COVID-19
This three-part series will examine the racial disparities in health brought vividly to public attention during the COVID-19 pandemic. The first panel in our series will explore the importance of collecting and utilizing data on race to better understand the impact of the pandemic.
Cohosted with Boston University Center for Antiracist Research
What you'll learn
At the end of the recording, participants will be able to:
- Describe economic effects of COVID on households included in the Children’s HealthWatch survey.
- Describe evidence for the association of structural racism and telehealth inequities among Black and Latinx communities, and the implications of those inequities
- List 2 factors experienced by Black and Latinx students that negatively influence their academic success and provide a possible intervention to address them
- Describe data limitations that impede comparing COVID case and death rates across States, as identified by the COVID Racial Data Tracker
Moderator
-

Sandro Galea
@sandrogaleaDean and Robert A. Knox Professor, Boston University School of Public Health

Ibram Kendi
@dribramDirector and Founder, Center for Antiracist Research, Boston University
Jayakanth Srinivasan
Research Associate Professor, Boston University Questrom School of Business

Megan Sandel
@megansandelAssociate Professor, Pediatrics, Boston University School of Medicine

Stephen A. Wilson
Chair, Family Medicine, Boston University School of Public Health

Aviva Geiger Schwarz
Data Editor, The COVID Racial Data Tracker, Boston University Center for Antiracist Research

Stephanie Ettinger de Cuba
@stephaniedc
Executive Director, Children’s HealthWatch

Kimberly Atkins
@kimberlyatkinsMODERATOR
Senior Opinion Writer,
The Boston Globe
Julia Raifman
@juliaraifmanAssistant Professor,
Boston University
School of Public Health
Kaye-Alese Green
@kayaleseDiversity & Inclusion Fellow, BUSM, Visiting Fellow, Institute of Health Systems Innovation & Policy
Sandro Galea, a physician, epidemiologist, and author, is dean and Robert A. Knox Professor at Boston University School of Public Health. He previously held academic and leadership positions at Columbia University, the University of Michigan, and the New York Academy of Medicine. He has published extensively in the peer-reviewed literature, and is a regular contributor to a range of public media, about the social causes of health, mental health, and the consequences of trauma. He has been listed as one of the most widely cited scholars in the social sciences. He is chair of the board of the Association of Schools and Programs of Public Health and past president of the Society for Epidemiologic Research and of the Interdisciplinary Association for Population Health Science. He is an elected member of the National Academy of Medicine. Galea has received several lifetime achievement awards. Galea holds a medical degree from the University of Toronto, graduate degrees from Harvard University and Columbia University, and an honorary doctorate from the University of Glasgow.
Subject Matter Experts
Ibram X. Kendi is the Andrew W. Mellon Professor in the Humanities at Boston University and the founding director of the BU Center for Antiracist Research. He is a contributing writer at The Atlantic and a CBS News correspondent. He is the author of many books including Stamped from the Beginning: The Definitive History of Racist Ideas in America, which won the National Book Award for Nonfiction, and four #1 New York Times bestsellers, How to Be an Antiracist; Stamped: Racism, Antiracism, and You, co-authored with Jason Reynolds; and Antiracist Baby, illustrated by Ashley Lukashevsky and Four Hundred Souls: A Community history of African America 1619-2019, edited with Keisha N. Blain. In 2020, Time magazine named him one of the 100 most influential people in the world.
Kimberly Atkins is a senior opinion writer and columnist at The Boston Globe, and lead columnist for The Emancipator, a joint venture by Globe Opinion and the Boston University Center for Antiracist Research that reimagines 19th-century abolitionist newspapers to reframe the current national conversation on racial justice. She is also an MSNBC contributor, and a guest host for the NPR/WBUR-produced news program On Point. She is also co-host of the weekly podcast #SistersInLaw, which breaks down the law behind the headlines of the week. Previously, Kimberly was the first Washington, DC-based news correspondent for WBUR. She has also served as the Boston Herald’s Washington bureau chief, guest host of C-SPAN’s morning call-in show Washington Journal, and a Supreme Court reporter for Massachusetts Lawyers Weekly and its sister publications. She has appeared as a political commentator on a host of national and international television and radio networks, including CNN, Fox News, NBC News, PBS, NPR, Sky News (UK), and CBC News (Canada). Before launching her journalism career, she was a trial and appellate litigation attorney in Boston. Kimberly is a native of Michigan, and a graduate of Wayne State University, Boston University School of Law and Boston University College of Communication, and the Columbia University Graduate School of Journalism.
Kaye-Alese Green received a BS in Psychology and Master’s in Interdisciplinary Studies with a dual concentration in Public Health and Urban Education from the University of Central Florida. Currently she is in between her second and third year of medical school and is serving as the inaugural Diversity & Inclusion Fellow for Boston University School of Medicine with a joint appointment as a Research Fellow at BU’s Institute of Health Systems Innovation & Policy. Ms. Green’s research interests include pediatric trauma, medical education reform and upstream divers of health disparities.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.

Antiracism as Health Policy (Part 2)
What are some of the flaws in
using race as a standalone measure of risk?


Register
Course Information
- Audience: Public Health Professionals
- Format: Webinar
- Date/Time: Tuesday, April 6th 2021, 4:30 PM – 6 PM EST.
- Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 1. Provider ID: 1131137 Event ID: SS1131137_AHP2.
If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Data Analytics and Assessment Skills
- Learning Level: Awareness
- Companion Trainings: Antiracism as Health Policy (Part 1)
Antiracism as Health Policy (Part 3) - Supplemental materials:None
- Pre-requisites: None
About this Recording
Part 2: Connecting research and policy
This three-part series will examine the racial disparities in health brought vividly to public attention during the COVID-19 pandemic. The second panel will focus on linking research to policy.
Cohosted with the Boston University Center for Antiracist Research and the Rockefeller Foundation-Boston University 3-D Commission.
What you'll learn
At the end of the recording, participants will be able to:
- List at least 5 social or health factors that were associated with race and risk of infection, illness, and death from COVID-19
- Discuss the role of data and analysis in advancing racial equity in the COVID-19 response
- List 6 areas of research on structural racism being conducted nationally
Moderator
-

Sandro Galea
@sandrogaleaDean and Robert A. Knox Professor, Boston University School of Public Health

Ibram Kendi
@dribramDirector and
Founder,
Center for Antiracist Research, Boston University
Ayanna Pressley
@AyannaPressleyAssociate Professor, Pediatrics, Boston University School of Medicine

Samantha Artiga
@sartiga2Vice President, Director, Disparities Policy Project, Kaiser Family Foundation

Patricia Williams
@nuslUniversity Distinguished Professor of Law and Humanities, Northeastern University School of Law

Laura Magaña
@lauramagvall(MODERATOR) President and CEO, Association of Schools and Programs of Public Health

Eliseo J. Pérez-Stable
@nimhdDirector of the National Institute on Minority Health and Health Disparities at the National Institutes of Health
Sandro Galea, a physician, epidemiologist, and author, is dean and Robert A. Knox Professor at Boston University School of Public Health. He previously held academic and leadership positions at Columbia University, the University of Michigan, and the New York Academy of Medicine. He has published extensively in the peer-reviewed literature, and is a regular contributor to a range of public media, about the social causes of health, mental health, and the consequences of trauma. He has been listed as one of the most widely cited scholars in the social sciences. He is chair of the board of the Association of Schools and Programs of Public Health and past president of the Society for Epidemiologic Research and of the Interdisciplinary Association for Population Health Science. He is an elected member of the National Academy of Medicine. Galea has received several lifetime achievement awards. Galea holds a medical degree from the University of Toronto, graduate degrees from Harvard University and Columbia University, and an honorary doctorate from the University of Glasgow.
Subject Matter Experts
Ibram X. Kendi is the Andrew W. Mellon Professor in the Humanities at Boston University and the founding director of the BU Center for Antiracist Research. He is a contributing writer at The Atlantic and a CBS News correspondent. He is the author of many books including Stamped from the Beginning: The Definitive History of Racist Ideas in America, which won the National Book Award for Nonfiction, and four #1 New York Times bestsellers, How to Be an Antiracist; Stamped: Racism, Antiracism, and You, co-authored with Jason Reynolds; and Antiracist Baby, illustrated by Ashley Lukashevsky and Four Hundred Souls: A Community history of African America 1619-2019, edited with Keisha N. Blain. In 2020, Time magazine named him one of the 100 most influential people in the world.
Congresswoman Ayanna Pressley is an activist, a legislator, a survivor, and the first woman of color to be elected to Congress from the Commonwealth of Massachusetts. Throughout her career as a public servant, Congresswoman Pressley has fought to ensure that those closest to the pain are closest to the power – driving and informing policymaking. Throughout her first term in Congress, Congresswoman Pressley has been a champion for justice: reproductive justice, justice for immigrants, consumer justice, justice for aging Americans, justice for workers, justice for survivors of sexual violence, and justice for the formerly and currently incarcerated. Currently, Congresswoman Pressley serves on two powerful Congressional committees – the House Committee on Oversight and Reform and the House Committee on Financial Services– both of which have remained focused on legislatively addressing issues of care, concern, and consequence to the American people. Prior to being elected to Congress, she served on the Boston City Council for 8 years, and was the first woman of color elected to the council in its 100-year history.
Samantha Artiga serves as Vice President and Director of the Racial Equity and Health Policy Program at KFF. In this role, Ms. Artiga leads KFF’s work to provide timely and reliable data, information, and policy analysis on health and health care disparities affecting people of color and underserved groups and efforts to advance racial equity in health and health care. Her work focuses on the intersection of racism and discrimination, social and economic inequities, and health. She also has conducted extensive work related to the health and health care needs of low-income populations and immigrant families and previously served as Associate Director of KFF’s Program on Medicaid and the Uninsured. Ms. Artiga holds a master’s degree in health policy from the George Washington University.
Professor Williams, one of the most provocative intellectuals in American law and a pioneer of both the law and literature and critical race theory movements in American legal theory, holds a joint appointment between the School of Law and the Department of Philosophy and Religion in the College of Social Sciences and Humanities. She is also director of Law, Technology and Ethics Initiatives in the School of Law and the College of Social Sciences and Humanities. Professor Williams has published widely in the areas of race, gender, literature and law. Her books, including The Alchemy of Race and Rights (Harvard University Press, 1991), illustrate some of America’s most complex societal problems and challenge our ideas about socio-legal constructs of race and gender. Her work remains at the cutting edge of legal scholarship. Drawing on her prior interrogation of race, gender and personhood, Professor Williams’ current research raises core questions of individual autonomy and identity in the context of legal and ethical debates on science and technology. Her work in the area of health and genetics, for example, questions how racial formation is shaped by the legal regulation of private industry and government. Her work on algorithms grapples with the auditing function of technology in our everyday lives — shaping how we understand who we are.
Dr. Laura Magaña joined the Association of Schools and Programs of Public Health (ASPPH) as President and CEO in August 2017. Under Dr. Magaña’s leadership, ASPPH has continued to advance its mission to strengthen the capacity of members by advancing leadership, excellence, and collaboration for academic public health. During her tenure, ASPPH has significantly grown its global engagement, launched the academic public health leadership institute, and enhanced the voice of academic public health through advocacy efforts. Prior to joining ASPPH, Dr. Magaña dedicated more than 35 years to successfully leading the transformation and advancements of public and private universities in Mexico; educational organizations in the USA; United Nations programs; and NGO’s in Central America and Europe. She was most recently the dean of the School of Public Health in Mexico at the ASPPH-member National Institute of Public Health (INSP). Her diverse portfolio features academic publications, educational technological developments many of which relate to learning environments, the use of technology in education, and public health education. She has also been a faculty member and lecturer in diverse universities around the world.
Eliseo J. Pérez-Stable, M.D. is Director of the National Institutes of Health’s National Institute on Minority Health and Health Disparities (NIMHD), which seeks to advance the science of minority health and health disparities research through research, training, research capacity development, public education, and information dissemination. Dr. Pérez-Stable practiced general internal medicine for 37 years at the University of California, San Francisco (UCSF) before moving to NIH in September 2015. He was professor of medicine at UCSF and chief of the Division of General Internal Medicine for 17 years. His research interests include improving the health of racial and ethnic minorities and underserved populations, advancing patient-centered care, improving cross-cultural communication skills among clinicians, and promoting diversity in the biomedical research workforce. For more than 30 years, Dr. Pérez-Stable led research on Latino smoking cessation and tobacco control policy in the United States and Latin America, addressing clinical and prevention issues in cancer screening, and mentoring over 70 minority investigators. He has published over 300 peer-reviewed articles and was elected to the National Academy of Medicine in 2001.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.

Antiracism as Health Policy (Part 3)
Why does
intersectionality matter when studying health disparities and how does this
relate to COVID susceptibilities among men and women of color?


Register
Course Information
- Audience: Public Health Professionals
- Format: Webinar
- Date/Time: Wednesday, April 7th 2021 4:30 PM – 6 PM EST.
- Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 1. Provider ID: 1131137 Event ID: SS1131137_AHP3.
If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Data Analytics and Assessment Skills
- Learning Level: Awareness
- Companion Trainings: Antiracism as Health Policy (Part 1)
Antiracism as Health Policy (Part 2) - Supplemental materials:None
- Pre-requisites: None
About this Recording
Part 3: Antiracist policy solutions
This three-part series will examine the racial disparities in health brought vividly to public attention during the COVID-19 pandemic. The third panel will conclude our series with examining antiracist policy solutions that are informed by data.
Cohosted with Boston University Center for Antiracist Research.
What you'll learn
At the end of the recording, participants will be able to:
- Describe the approach and requirements of the Anti-Racism in Public Health Act of 2020, introduced in September 2020
- Describe three essential elements of antiracist health policy solutions
- Discuss importance of intersectional antiracism research and practice
- Discuss lessons learned from the COVID experience in New York City about an antiracist approach to public health emergencies
- Describe a framework for advancing health equity through policies for care delivery and payment reform
Moderator
-

Sandro Galea
@sandrogaleaDean and Robert A. Knox Professor, Boston University School of Public Health

Ibram Kendi
@dribramDirector andFounder,
Center for Antiracist Research, Boston University
Elizabeth Warren
@senwarren(OPENING CONVERSATION)
U.S. Senate, Massachusetts
Dustin Duncan
@drdustinduncanAssociate Professor of Epidemiology, Columbia Mailman School of Public Health

Torian Easterling
@drtorianFirst Deputy Commissioner and Chief Equity Officer, NYC Department of Health and Mental Hygiene

Regina Davis Moss
@dr4equity(MODERATOR)
Associate Executive Director, American Public Health Association
Consuelo H. Wilkins
@drchwilkinsProfessor of Medicine, Vice President for Health Equity, Associate Dean for Health Equity, Vanderbilt University Medical Center

Marshall Chin
@marshallchinmdChair, Family Medicine,
Boston University
School of
Public Health
Sandro Galea, a physician, epidemiologist, and author, is dean and Robert A. Knox Professor at Boston University School of Public Health. He previously held academic and leadership positions at Columbia University, the University of Michigan, and the New York Academy of Medicine. He has published extensively in the peer-reviewed literature, and is a regular contributor to a range of public media, about the social causes of health, mental health, and the consequences of trauma. He has been listed as one of the most widely cited scholars in the social sciences. He is chair of the board of the Association of Schools and Programs of Public Health and past president of the Society for Epidemiologic Research and of the Interdisciplinary Association for Population Health Science. He is an elected member of the National Academy of Medicine. Galea has received several lifetime achievement awards. Galea holds a medical degree from the University of Toronto, graduate degrees from Harvard University and Columbia University, and an honorary doctorate from the University of Glasgow.
Subject Matter Experts
Ibram X. Kendi is the Andrew W. Mellon Professor in the Humanities at Boston University and the founding director of the BU Center for Antiracist Research. He is a contributing writer at The Atlantic and a CBS News correspondent. He is the author of many books including Stamped from the Beginning: The Definitive History of Racist Ideas in America, which won the National Book Award for Nonfiction, and four #1 New York Times bestsellers, How to Be an Antiracist; Stamped: Racism, Antiracism, and You, co-authored with Jason Reynolds; and Antiracist Baby, illustrated by Ashley Lukashevsky and Four Hundred Souls: A Community history of African America 1619-2019, edited with Keisha N. Blain. In 2020, Time magazine named him one of the 100 most influential people in the world.
Elizabeth Warren, a fearless consumer advocate who has made her life’s work the fight for middle class families, was elected to the United States Senate on November 6, 2012, by the people of Massachusetts. Elizabeth is recognized as one of the nation’s top experts on bankruptcy and the financial pressures facing middle class families, and the Boston Globe has called her “the plainspoken voice of people getting crushed by so many predatory lenders and under regulated banks.” She is widely credited for the original thinking, political courage, and relentless persistence that led to the creation of the Consumer Financial Protection Bureau. President Obama asked her to set up the new agency to hold Wall Street banks and other financial institutions accountable, and to protect consumers from financial tricks and traps often hidden in mortgages, credit cards and other financial products. In the aftermath of the 2008 financial crisis, Warren served as Chair of the Congressional Oversight Panel for the Troubled Asset Relief Program (TARP). Her independent and tireless efforts to protect taxpayers, to hold Wall Street accountable, and to ensure tough oversight of both the Bush and Obama Administrations won praise from both sides of the aisle. The Boston Globe named Elizabeth Warren Bostonian of the Year and TIME Magazine called her a “New Sheriff of Wall Street” for her oversight efforts. During her campaign for the Senate, Elizabeth promised to fight for middle class families and to make sure that everyone has a fair shot to get ahead. She called for policies that would level the regulatory playing field for small businesses and ensure that everyone – even large and powerful corporations – pays a fair share in taxes and is held accountable for breaking the law. Endorsing Elizabeth’s candidacy, the New Bedford Standard-Times said, “Elizabeth Warren has it right on all the things that matter most to us in SouthCoast and across Massachusetts,” with “principles that without a doubt, promote the well-being of the middle class.” The Boston Globe called Elizabeth “a fierce advocate for the lot of working families, creating educational opportunities, and expanding medical research.” The Springfield Republican said, “We need a voice for working families in Washington again. Elizabeth Warren will give us that voice.” Senator Warren was a law professor for more than 30 years, including nearly 20 years as the Leo Gottlieb Professor of Law at Harvard Law School. The graduating class at Harvard twice recognized her with the Sacks-Freund Award for excellence in teaching. She taught courses on commercial law, contracts, and bankruptcy and wrote more than a hundred articles and ten books, including three national best-sellers, A Fighting Chance, The Two-Income Trap, and All Your Worth. National Law Journal named her one of the Most Influential Lawyers of the Decade, TIME Magazine has named her one of the 100 most influential people in the world four times, and she has been honored by the Massachusetts Women’s Bar Association with the Lelia J. Robinson Award. Elizabeth learned first-hand about the economic pressures facing working families, growing up in a family she says was “on the ragged edge of the middle class.” She got married at 19, and after graduating from college, started teaching in elementary school. Her first baby, a daughter Amelia, was born when Elizabeth was 22. When Amelia was two, Elizabeth started law school. Shortly after she graduated, her son Alex was born. Elizabeth hung out a shingle and practiced law out of her living room, but she soon returned to teaching. Elizabeth is a graduate of the University of Houston and Rutgers School of Law. Elizabeth and her husband Bruce Mann have been married for 38 years and live in Cambridge, Massachusetts with their golden retriever, Bailey. They have three grandchildren.
Dustin T. Duncan, ScD is an Associate Professor in the Department of Epidemiology at Columbia University Mailman School of Public Health, where he directs Columbia’s Spatial Epidemiology Lab and co-directs the department’s Social and Spatial Epidemiology Unit. Dr. Duncan is a Social and Spatial Epidemiologist. Dr. Duncan’s intersectional research focuses on Black gay, bisexual and other sexual minority men and transgender women of color. His work appears in leading public health, epidemiology, medical, geography, criminology, demography, and psychology journals. Working in collaborations with scholars across the world, he has over 150 high-impact articles, book chapters and books, and his research has appeared in major media outlets including U.S. News & World Report, The Washington Post, The New York Times and CNN. Dr. Duncan’s recent work has been funded by the National Institutes of Health, the Centers for Disease Control and Prevention, the HIV Prevention Trials Network, the Robert Wood Johnson Foundation, the Verizon Foundation, and the Aetna Foundation. He has received several early career and distinguished scientific contribution awards including from the Harvard University T.H. Chan School of Public Health and the Interdisciplinary Association for Population Health Science (IAPHS). In 2020, he received the Mentor of the Year Award from Columbia University Irving Medical Center’s Irving Institute for Clinical and Translational Research.
Dr. Easterling serves as the First Deputy Commissioner and Chief Equity Officer at the NYC Department of Health and Mental Hygiene (NYCDOHMH). Dr. Easterling has spent more than 5 years in a senior leadership role at the Health Department. Prior to serving as First Deputy Commissioner and Chief Equity Officer, Dr. Easterling served as Deputy Commissioner of the Center for Health Equity and Community Wellness at the NYC DOHMH, where he oversaw programmatic work focused on reducing overall premature mortality and closing the racial gap on the top leading causes of preventable death. He also served as the Assistant Commissioner of the Department of Health’s Bureau of Brooklyn Neighborhood Health, where he helped advance key programming to address pressing concerns, including maternal deaths and gun violence. Dr. Easterling is a community physician committed to health equity, social justice and movement building to achieve the health outcomes that all people deserve both locally and globally. Dr. Easterling holds a Bachelor of Science from Morehouse College (Atlanta, GA), a Doctor of Medicine (M.D.) from Rutgers-New Jersey Medical School, and a Master of Public Health (M.P.H) from Icahn School of Medicine at Sinai in New York. He completed his residency in Family Medicine at Jamaica Hospital Medical Center in Queens, NY and a General Preventive Medicine residency at Icahn School of Medicine at Sinai in New York.
Regina Davis Moss is the associate executive director of the American Public Health Association. She oversees a broad portfolio of programs addressing the social determinants of health and has nearly 20 years of experience managing national health promotion initiatives addressing health equity, women’s health, and public health system capacity building. Formerly, Dr. Davis Moss held a senior management position for a chronic disease prevention effort for the National Institute of Health. Prior to that, she worked for the Kaiser Family Foundation where she helped launch the Kaiser Health News online information service and served as the senior producer. Dr. Davis Moss came to Kaiser after serving as a supervisor for an epidemiologic study focused on women’s reproductive health. She also served as a public health service fellow in the Office on Women’s Health for the U.S. Department of Health and Human Services. Dr. Davis Moss earned her Ph.D. in Maternal and Child Health from the University of Maryland, College Park; M.P.H. from George Washington University; B.S. from Howard University, and certificate in public health performance improvement from the University of Minnesota.
Consuelo H. Wilkins, MD, MSCI, Professor of Medicine, Vice President for Health Equity and Associate Dean for Health Equity, Vanderbilt University Medical Center, is a nationally recognized thought leader in health equity and in addressing the elimination of systemic inequities that impact the health and well-being of racial/ethnic minorities. As a community engagement research scientist, Dr. Wilkins has pioneered new approaches to engaging vulnerable, socioeconomically disadvantaged, and minority populations. She is Principal Investigator of three NIH-funded centers, the Vanderbilt-Miami-Meharry Center of Excellence in Precision Medicine and Population Health; the Center for Improving Clinical Trial Education Recruitment and Enrollment at CTSA Hubs; and the Vanderbilt Institute for Clinical and Translational Research. She is also PI of a Robert Wood Johnson Foundation award on engendering trust in health care among African American men. Dr. Wilkins earned a Bachelor of Science in microbiology and Doctor of Medicine from Howard University. She completed a residency in Internal Medicine at Duke University Medical Center and a Geriatric Medicine fellowship at Washington University School of Medicine/Barnes-Jewish Hospital. Following her medical training, she earned a Master of Science in Clinical Investigation from Washington University School of Medicine.
Marshall Chin, MD, MPH, is a general internist with extensive experience improving the care of vulnerable patients with chronic disease. He has worked to advance diabetes care and outcomes on the South Side through health care system and community interventions. He also leads initiatives to improve health strategies at a national level as director of the Robert Wood Johnson Foundation (RWJF)’s Finding Answers: Solving Disparities Through Payment and Delivery System Reform Program Office and Co-Director of the Merck Foundation’s Bridging the Gap: Reducing Disparities in Diabetes Care National Program Office. Dr. Chin performed many of the key research studies informing how to improve diabetes care and outcomes in federally-qualified health centers serving vulnerable populations with limited resources. His work over the past decade leading RWJF’s Finding Answers program led to the creation of the Roadmap to Reduce Disparities. Current projects include improving diabetes outcomes in real-world settings, reducing health disparities by transforming the way care is organized and paid for, enhancing care by facilitating partnerships between the health care system and other sectors such as food and housing, and improving shared decision making among clinicians and LGBTQ people of color. In addition to his clinical and research roles, Dr. Chin is a teacher and award-winning mentor, committed to providing opportunities for trainees. As co-director of the Summer Program in Outcomes Research Training (SPORT), Dr. Chin educates faculty, fellows and students about outcomes research methods — to better understand and improve quality of care. An expert in health care disparities in medicine, Dr. Chin frequently is invited to present his work at national conferences and serve on policy committees. He serves on the National Institute on Minority Health and Health Disparities National Advisory Council and Centers for Disease Control and Prevention (CDC) Community Preventive Services Task Force. He co-chairs the National Quality Forum (NQF) Disparities Standing Committee and is a former President of the Society of General Internal Medicine (SGIM). Dr. Chin was elected to the National Academy of Medicine in 2017.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.


Biography of Resistance: The Epic Battle Between People and Pathogens
Learn more about this seminar!
Biography of Resistance: The Epic Battle Between People and Pathogens
Harmful strains of bacteria have resulted in plagues and pandemics for millennia. How are the driving forces of antibiotic resistance, and individual and societal decisions contributing to this developing public health crisis?


Register
Course Information
- Audience: Public health workforce audiences interested in antibiotic resistance
- Format: Webinar
- Date/Time: Recorded Wednesday, September 23, 2020 4:30 PM -6:00 PM ET
- Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hour. Maximum advanced-level continuing education contact hour is 1. Provider ID: SS1131137, Event ID: SS1131137_BREBBPP. If you are not seeking CHES/MCHES contact hours, if you complete the evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Public Health Sciences Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials: NA
- Pre-requisites: None
About this Seminar
Harmful strains of bacteria have resulted in plagues and pandemics for millennia. How are the driving forces of antibiotic resistance, and individual and societal decisions contributing to this developing public health crisis?
Note: This seminar was developed and recorded by BUSPH. Our Dean’s Signature Programs bring speakers to our campus to engage in thoughtful conversations about the pressing issues of public health. They are open to our entire community, designed to inform, stimulate, and encourage groundbreaking discussion.
What you'll learn
At the end of the seminar, participants will be able to:
- Describe the historical contributions of at least 5 researchers to the understanding of infectious disease
- List 4 ways in which global conflict contributes to increasing the occurrence of infectious diseases
- Describe the roles of agricultural practices and poverty in the occurrence of infectious diseases
- Identify market and economic concerns that negatively influence the generation of new anti-microbial drugs
Subject Matter Expert

Muhammad Zaman
Professor of Biomedical Engineering and International Health

Karen Weintraub
Health
and
Science Journalist
Muhammad H. Zaman is Howard Hughes Medical Institute Professor of Biomedical Engineering and International Health at Boston University. Prof. Zaman’s current research is focused on three areas, namely using quantitative tools to understand tumor metastasis, developing robust technologies for high-value healthcare problems in the developing world, particularly in the area of maternal and child health, and working on health and innovation policy issues in developing nations. Technologies developed by Prof. Zaman are in various stages of implementation in several countries. In 2013, Scientific American named a technology from Zaman’s lab, PharmaChk, among the 10 technologies that will change the world.
He has won numerous awards for his research and teaching from IEEE, FEBS, American Society for Engineering Education, USAID, The US National Academy of Sciences, The University of Texas System, Boston University and other national and international organizations. Most recently, he was named Howard Hughes Professor by the Howard Hughes Medical Institute and was elected as a Fellow of American Institute of Biological and Medical Engineering.
In addition to his research, Prof. Zaman is actively engaged in bringing quality engineering education in several developing nations. He is currently involved in setting up biomedical engineering departments at universities in Kenya, Zambia, Uganda and Ethiopia. He is Co-Director of the UN Africa Biomedical Initiative. He is a regular contributor on issues of drug quality control and global health for the Project Syndicate (his columns have appeared in newspapers in more than 20 countries) and Huffington Post, and writes a weekly column on innovation in health and education for leading Pakistan daily, Express Tribune, which is part of the International New York Times group.
Independent Health/Science journalist covering the biological sciences.Regular contributor to The New York Times, The Washington Post, Scientific American.com, WBUR radio and others. Journalism educator and book author.
Registration
Select the Enroll Me button below to register for this seminar recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
* Yale School of Public Health, Office of Public Health Practice, a New England Public Health Training Center partner, is a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. All CHES credit inquiries are managed by YSPH

Centering the Health of Mothers in the Public Health Agenda
How do we put the needs of mothers at the heart of public health?


Register
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Monday, October 24, 2022, 1:00 PM – 2:30 PM ET
- Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1.5 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_CHMPHA.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Health Equity Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
Approximately 4 million women give birth each year in the U.S. Yet, traditional public health approaches have continued to consider maternal and child health together. How do we put the needs of mothers at the heart of public health? And how do we ensure attention to the health of all persons who give birth?
What you'll learn
At the end of the recording, participants will be able to:
- Describe the limited reproductive choices that black women, women of color, and immigrant women have due to structural racism.
- Define reproductive justice and discuss the right of all people to have or not have children under safe conditions.
- Discuss the need for culturally and linguistically appropriate healthcare for achieving reproductive autonomy.
- Analyze the role popular visual culture has in depicting the fetus and the pregnant body.
- Assess the maternal mental health difficulties during the perinatal period and identify the impacts this has on fetal health.
- Discuss how campaigns and interventions used in the UK can be applied to the U.S. to improve maternal mental health outcomes.
Moderator

Priyanka Dayal McCluskey
@PRIYANKA_DAYAL
Senior Health Reporter, WBUR
Marcela Howell
@BLACKWOMENSRJ
President; CEO, In Our Own Voice: National Black Women's Reproductive Justice Agenda
May Sudhinaraset
@UCLAFSPH
Associate Professor, University of California Los Angeles Fielding School of Public Health
Monica McLemore
@MCLEMOREMR
Professor, Interim Director, Center for Anti-Racism in Nursing University of Washington, School of Nursing
Elizabeth Armstrong
@PRINCETON
Head of Butler College, Associate Professor of Sociology and Public Affairs, Princeton University
Fiona Challacombe
@DRFIONACH
NIHR Clinical
Lecturer,
Kings College London
Priyanka Dayal McCluskey is a senior health reporter for WBUR, Boston’s NPR news station. Her work airs on the radio and appears online at WBUR.org. Before joining WBUR in 2022, she spent eight years as a health care reporter at The Boston Globe. She previously covered health and medicine at the Boston Herald. She began her career writing local news for the Worcester Telegram & Gazette. Priyanka’s coverage spans health business and policy, medical research, and health disparities. She is focused on how the health care system serves — and doesn’t serve — patients. Her recent work chronicles the impact of the COVID-19 pandemic on patients, workers, and the health care system. She is a co-author of WBUR’s CommonHealth newsletter. Priyanka has a B.S. in Journalism and a B.A. in Political Science from Boston University.
Subject Matter Experts
Marcela Howell is the president & CEO of In Our Own Voice: National Black Women’s Reproductive Justice Agenda, a national-state partnership with eight Black women’s Reproductive Justice organizations with a goal of lifting up the voices of Black leaders on reproductive rights, health and justice. An advocate and policy strategist, Marcela is recognized for her expertise in strategic communications, leadership development and policy forecasting. With over 40 years of experience advocating for reproductive justice and women’s empowerment, she is devoted to enhancing the role of Black women in national policy debates on issues that impact their lives. Marcela has testified before Congress on abortion access, reproductive rights and justice and the empowerment of Black women and has been quoted in numerous publications, including Newsweek, Washington Post, Ms. Magazine, Blavity, and Essence Magazine. Marcela is the author of Walk in My Shoes: A Black Activist’s Guide to Surviving the Women’s Movement, a collection of inspirational essays to help young Black women navigate the women’s movement and empower them to become leaders in the fight for reproductive justice.
Dr. May Sudhinaraset, PhD is an Associate Professor in Community Health Sciences in the School of Public Health at UCLA. She is trained as a social epidemiologist from Johns Hopkins Bloomberg School of Public Health. Her research focuses on understanding the social determinants of migrant, adolescent, and women’s health both globally and in the US. Her work centers around three complementary streams of work: (1) social and cultural contexts of vulnerable adolescents and women; (2) global women’s health and quality of service delivery; and (3) social policies and immigration in the US. Her global work includes women’s experiences during childbirth, family planning, and abortion services, development of quality improvement interventions in Kenya and India, and large-scale maternal and child health evaluations in Myanmar. She currently is Principal Investigator of the BRAVE Study (Bridging communities Raising API Voices for health Equity), the first study to assess the health status and health care utilization of undocumented Asian and Pacific Islander young adults. Using community participatory approaches, this study explores the impact of social policies, including Deferred Action for Childhood Arrivals, on the social and health outcomes of undocumented young adults. She has collaborated with institutions and researchers in Myanmar, Kenya, India, Thailand and China.
Dr. Monica R. McLemore is a tenured professor in the Child, Family, and Population Health Department and the Interim Director for the Center for Anti-Racism in Nursing at the University of Washington School of Nursing. Prior to her arrival at UW, she was a tenured associate professor at the University of California, San Francisco and was named the Thelma Shobe Endowed Chair in 2021. She retired from clinical practice as a public health and staff nurse after a 28-year clinical nursing career in 2019, however, continues to provide flu and COVID-19 vaccines. Her program of research is focused on understanding reproductive health and justice. To date, she has 93 peer reviewed articles, OpEds and commentaries and her research has been cited in the Huffington Post, Lavender Health, five amicus briefs to the Supreme Court of the United States, and three National Academies of Science, Engineering, and Medicine reports, and a data visualization project entitled How To Fix Maternal Mortality: The first step is to stop blaming women that was published in the 2019 Future of Medicine edition of Scientific American. Her work has also appeared in publications such as Dame Magazine, Politico, ProPublica/NPR and she made a voice appearance in Terrance Nance’s HBO series Random Acts of Flyness. She is the recipient of numerous awards and currently serves as chair for Sexual and Reproductive Health section of the American Public Health Association. She was inducted as a fellow of the American Academy of Nursing in 2019. She became the Editor in Chief of Health Equity Journal in 2022.
Elizabeth M Armstrong is an Associate Professor in the Department of Sociology with joint affiliations in The Princeton School of Public and International Affairs and the Office of Population Research. Her research interests include public health, the history and sociology of medicine, risk in obstetrics, and medical ethics. She is currently conducting research on diseases and agenda-setting, and on fetal personhood and the evolution of obstetrical practice and ethics. She is the author or coauthor of articles in Health Affairs, Social Science and Medicine, Journal of Marriage and the Family, International Family Planning Perspectives, and Studies in Family Planning and is the author of Conceiving Risk, Bearing Responsibility: Fetal Alcohol Syndrome and the Diagnosis of Moral Disorder (Johns Hopkins University Press, 2003). She was a Robert Wood Johnson Foundation Scholar in Health Policy Research at the University of Michigan from 1998-2000. Ph.D. University of Pennsylvania.
Dr. Challacombe qualified as a clinical psychologist from the IOPPN, King’s College London in 2005. After working in clinical practice she gained a Peggy Pollak research fellowship from the Psychiatry Research Trust and completed a PhD at King’s College London in 2014. Her research examined the impact of perinatal obsessive-compulsive disorder on women and children. She conducted the first randomised controlled trial of CBT for postpartum OCD, investigating treatment effects on anxiety and parenting. She joined the Section of Women’s Mental Health at the IOPPN in 2017 and gained an NIHR fellowship to investigate treatments for perinatal anxiety disorders in 2018. She is a senior clinician at the Maudsley Centre for Anxiety Disorders and Trauma (CADAT) where she has developed and leads a sub-service for parents with anxiety disorders. She is author of the self-help book Break Free from OCD and a therapist treatment manual CBT for OCD.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of award 2 UB6HP31685‐05‐00 “Public Health Training Centers.” The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government.

Challenging Public Health: Michelle Holder
How did COVID highlight and exacerbate economic and employment conditions disproportionately among women and persons of color? What can we learn to change those conditions as we move forward?


Register
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Tuesday, April 5th, 2022 1:00 PM – 2:00 PM EST
- Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_CPHMH.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Health Equity Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
Our Challenging Public Health series invites speakers from outside of public health to reflect on the public health response to the COVID-19 pandemic. This conversation features Michelle Holder, President and CEO of the Washington Center for Equitable Growth. Holder’s research focuses primarily on how the US job market discriminates against people of color, particularly Black women, who not only face a gender wage gap but a racial wage gap. She has written extensively on this subject, including The ‘Double Gap’ and the Bottom Line: African American Women’s Wage Gap and Corporate Profits, and more recently The Early Impact of Covid-19 on Job losses among Black Women in the United States.
What you'll learn
At the end of the recording, participants will be able to:
- Describe how the public health system underperformed during COVID from policy and political perspectives
- Discuss evidence for disparate effects of COVID on job loss and negative economic effects across gender, race, and class lines
- Discuss lessons learned to improve public health response to combat more effectively the disparate outcomes of COVID along racial and ethnic lines
Moderator

Sandro Galea
@SANDROGALEA
MODERATOR Dean and Robert A Knox Professor, Boston University School of Public Health

Michelle Holder
President of the Washington Center for Equitable Growth; Associate Professor of Economics, John Jay College, City University of New York
@MLHOLDER999
Sandro Galea, a physician, epidemiologist, and author, is dean and Robert A. Knox Professor at Boston University School of Public Health. He previously held academic and leadership positions at Columbia University, the University of Michigan, and the New York Academy of Medicine. He has published extensively in the peer-reviewed literature, and is a regular contributor to a range of public media, about the social causes of health, mental health, and the consequences of trauma. He has been listed as one of the most widely cited scholars in the social sciences. He is past chair of the board of the Association of Schools and Programs of Public Health and past president of the Society for Epidemiologic Research and of the Interdisciplinary Association for Population Health Science. He is an elected member of the National Academy of Medicine. Galea has received several lifetime achievement awards. Galea holds a medical degree from the University of Toronto, graduate degrees from Harvard University and Columbia University, and an honorary doctorate from the University of Glasgow.
Subject Matter Expert
Michelle Holder is President and CEO of the Washington Center for Equitable Growth as well as Associate Professor of Economics at John Jay College, City University of New York. Prior to joining the John Jay College faculty, she worked as an applied economist for a decade in both the nonprofit and government sectors. Her research focuses on the Black community and women of color in the American labor market, and her economic policy reports have been covered by the New York Times, the Wall Street Journal, the New York Amsterdam News, El Diario, and Dollars & Sense magazine. Michelle has also appeared on, or been quoted in, media outlets such as CNN, the Washington Post, NPR, The New Yorker, Black News Channel (BNC), PBS, MSNBC, Al Jazeera-English, Marketplace, and Vox.com. Her second book, Afro-Latinos in the U.S. Economy, co-authored with Alan Aja, was released May 2021 by Lexington Books, an imprint of Rowman & Littlefield. Michelle received M.A. and Ph.D. degrees in economics from The New School for Social Research, and a bachelor’s degree in economics from Fordham University.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.

Challenging Public Health: Rebecca Traister
How can anger about inequities be channeled into effective activism for social change?


Register
Course Information
- Audience: Public Health Professionals
- Format: Webinar
- Date/Time: Tuesday, February 1st, 2022 1:00 PM – 2:00 PM EST
- Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_CPHRT.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Data Analytics and Assessment Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
Our Challenging Public Health series invites speakers from outside of public health to reflect on the public health response to the COVID-19 pandemic. This conversation features Rebecca Traister, writer at large for New York magazine and author of Good and Mad, All the Single Ladies, and Big Girls Don’t Cry discussing her perspectives on how public health can do better.
What you'll learn
At the end of the recording, participants will be able to:
- Describe how inequitable social policies that influence the health of the public were highlighted in the pandemic
- Discuss the role of journalists and how public health professionals can effectively interact with them in moving policies that shape public health
- Discuss the role of state and federal politics in the future of public health
Moderator

Sandro Galea
@SANDROGALEA
MODERATOR Dean and Robert A Knox Professor, Boston University School of Public Health

Rebecca Traister
Writer at Large, New York Magazine
@RTRAISTER
Sandro Galea, a physician, epidemiologist, and author, is dean and Robert A. Knox Professor at Boston University School of Public Health. He previously held academic and leadership positions at Columbia University, the University of Michigan, and the New York Academy of Medicine. He has published extensively in the peer-reviewed literature, and is a regular contributor to a range of public media, about the social causes of health, mental health, and the consequences of trauma. He has been listed as one of the most widely cited scholars in the social sciences. He is past chair of the board of the Association of Schools and Programs of Public Health and past president of the Society for Epidemiologic Research and of the Interdisciplinary Association for Population Health Science. He is an elected member of the National Academy of Medicine. Galea has received several lifetime achievement awards. Galea holds a medical degree from the University of Toronto, graduate degrees from Harvard University and Columbia University, and an honorary doctorate from the University of Glasgow.
Subject Matter Expert
REBECCA TRAISTER is writer at large for New York magazine. A National Magazine Award winner, she has written about women in politics, media, and entertainment from a feminist perspective for The New Republic and Salon and has also contributed to The Nation, The New York Observer, The New York Times and The Washington Post. She is the author of Good and Mad and All the Single Ladies, both New York Times best-sellers, and the award-winning Big Girls Don’t Cry. She lives in New York with her family.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.

Challenging Public Health: Saru Jayaraman
Only 7 states have legislation that requires full minimum wages for tipped restaurant workers. What will it take to change the laws in the other 43 states that will improve compensation for restaurant workers to be paid a livable wage? How does improving compensation for restaurant workers enhance public health?


Register
Course Information
- Audience: Public Health Professionals
- Format: Webinar
- Date/Time: Wednesday, March 23rd, 2022 1:00 PM – 2:00 PM EST
- Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_CPHSJ.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Data Analytics and Assessment Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
Our Challenging Public Health series invites speakers from outside of public health to reflect on the public health response to the COVID-19 pandemic. This conversation features Saru Jayaraman, lawyer, activist, and founder of One Fair Wage. Jayaraman has written several books exposing the challenges faced by restaurant workers, including Behind the Kitchen Door: The People Who Make and Serve Your Food and Forked: A New Standard for American Dining.
What you'll learn
At the end of the recording, participants will be able to:
- Discuss the primary concerns of restaurant workers, and how they were highlighted and exacerbated during the pandemic, making restaurants the #1 most dangerous places to work during the pandemic (per CDC)
- Describe current advocacy efforts to improve the wage structure for tipped restaurant workers to include full minimum wage plus tips
Moderator

Sandro Galea
@SANDROGALEA
MODERATOR Dean and Robert A Knox Professor, Boston University School of Public Health

Saru Jayaraman
@SARUJAYARAMAN
President, One Fair Wage
Sandro Galea, a physician, epidemiologist, and author, is dean and Robert A. Knox Professor at Boston University School of Public Health. He previously held academic and leadership positions at Columbia University, the University of Michigan, and the New York Academy of Medicine. He has published extensively in the peer-reviewed literature, and is a regular contributor to a range of public media, about the social causes of health, mental health, and the consequences of trauma. He has been listed as one of the most widely cited scholars in the social sciences. He is past chair of the board of the Association of Schools and Programs of Public Health and past president of the Society for Epidemiologic Research and of the Interdisciplinary Association for Population Health Science. He is an elected member of the National Academy of Medicine. Galea has received several lifetime achievement awards. Galea holds a medical degree from the University of Toronto, graduate degrees from Harvard University and Columbia University, and an honorary doctorate from the University of Glasgow.
Subject Matter Expert
Saru Jayaraman is the President of One Fair Wage and Director of the Food Labor Research Center at University of California, Berkeley. After 9/11, together with displaced World Trade Center workers, she co-founded the Restaurant Opportunities Center (ROC), which grew into a national movement of restaurant workers, employers and consumers. She then launched One Fair Wage as a national campaign to end all subminimum wages in the United States. Saru is a graduate of Yale Law School and the Harvard Kennedy School of Government. She was listed in CNN’s “Top10 Visionary Women” and recognized as a Champion of Change by the White House in 2014, a James Beard Foundation Leadership Award in 2015, and the SF Chronicle ‘Visionary of the Year’ in 2019. Saru is also the author of four books including the forthcoming, One Fair Wage: Ending All Subminimum Pay in America (The New Press, November 2021). Additional publications include Behind the Kitchen Door (Cornell University Press, 2013), Forked: A New Standard for American Dining (Oxford University Press, 2016), and Bite Back: People Taking on Corporate Food and Winning, (UC Press, 2020). She has appeared on MSNBC, HBO, PBS, CBS, and CNN. She attended the Golden Globes in January 2018 with Amy Poehler as part of the Times Up action to address sexual harassment.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.

Climate and Health: What can we do today? Session I
How can public health practitioners communicate accurate information about climate change to individuals and communities to motivate action?


Register
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Friday, March 18th, 2022
9:00 AM – 9:45 AM EST - Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_CH1.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Leadership and Systems Thinking
- Learning Level: Awareness
- Companion Trainings: Climate and Health: What can we do today? Session II
Climate and Health: What can we do today? Session III - Supplemental materials:None
- Pre-requisites: None
About this Recording
Recent heat waves, wildfires, hurricanes, and other extreme weather events around the world underscore that climate change represents a clear and present danger. Communities everywhere need to better prepare for the extreme weather events we are experiencing today. But how does a community do this?
What you'll learn
At the end of the recording, participants will be able to:
- Discuss intervention activities that can and should be done immediately for short-term and long-term impact
- Describe connections between climate change impacts and social determinants of health resulting in health disparities
- List 5 environmental potential contributors to adverse effects on the mental health of young people
- Define the roles and responsibilities of the new federal Office of Climate Change and Health Equity
Moderator

Greg Wellenius
@GWELLENIUS
Professor, Boston University School of Public Health
John Balbus
@DRJBALBUS
Interim Director, Office of Climate Change and Health Equity, US Department of Health and Human Services
Gregory Wellenius, ScD leverages his training in epidemiology, environmental health, and human physiology to lead research focused on assessing the human health impacts of the built environment in the context of a rapidly changing climate. His team has made a number of notable contributions to our understanding of the health risks associated with air pollution, noise pollution, other features of our physical environment, and those posed by a changing climate. A key goal of his team’s research is to provide the actionable scientific evidence needed to ensure that our communities are as resilient, sustainable, and healthy as possible, emphasizing the benefits to human health of climate change mitigation and adaptation efforts. Before coming to Boston University, Dr. Wellenius served as faculty and Director of Brown University’s Center for Environmental Health and Technology and Elected Councilor of the International Society for Environmental Epidemiology (ISEE). He has previously taught courses on epidemiology methods, climate change and human health, and methods in environmental epidemiology. He has a strong track record of mentoring undergraduate students, graduate students and post-doctoral fellows. Dr. Wellenius is the 2019 recipient of the ISEE Tony McMichael Mid-Term Career Award and the 2018 recipient of the Dean’s Award for Excellence in Teaching from the Brown University School of Public Health.
Subject Matter Expert
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.

Climate and Health: What can we do today? Session II
How can community-based organizations work effectively with academic institutions to address the effects of climate change in their communities?


Register
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Friday, March 18th, 2022
10:00 AM – 11:30 AM EST - Price: Free
- Length: 1.5 hours
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1.5 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_CH2.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Leadership and Systems Thinking
- Learning Level: Awareness
- Companion Trainings: Climate and Health: What can we do today? Session I Climate and Health: What can we do today? Session III
- Supplemental materials:None
- Pre-requisites: None
About this Recording
Recent heat waves, wildfires, hurricanes, and other extreme weather events around the world underscore that climate change represents a clear and present danger. Communities everywhere need to better prepare for the extreme weather events we are experiencing today. But how does a community do this?
What you'll learn
At the end of the recording, participants will be able to:
- Describe effective advocacy strategies employed by a community group (GreenRoots in Chelsea/East Boston) to address air quality and other environmental concerns
- List 4 principles to promote climate justice (i.e., address climate adaption for vulnerable people in vulnerable places)
- Describe 4 examples of actions that that US cities can take to address climate change
- Describe the goals, activities, and achievements of the Extreme Heat Resilience Alliance (EHRA)
- Explain research approach and methodologies to understand how housing characteristics are related to health impacts of heat among vulnerable populations
Moderator

Amruta Nori-Sarma
@ASANSREASON
Assistant Professor, Boston University School of Public Health
Marie S. O'Neill
Professor,
Department of Epidemiology,
University of Michigan

Kathy Baughman McLeod
@KBMCLEODFLA
Director, Adrienne Arsht-Rockefeller Foundation Resilience Center, Senior Vice President Atlantic Council
Sharon Harlan
Professor and Department Chair, Department of Health Sciences,
Northeastern University

Roseann Bongiovanni (CAS’99, SPH’01)
@GREENROOTSEJ
Executive Director, GreenRoots
Amruta Nori-Sarma is an Assistant Professor in the Environmental Health Department at Boston University School of Public Health, where she studies the relationship between environmental exposures associated with climate change and health outcomes in vulnerable communities. Her previous work has examined the impact of heat waves and air pollution on health in vulnerable communities in India, South Korea, and across the US. Her current research aims to understand the impacts of interrelated extreme weather events on mental health across the US utilizing large claims datasets. She also has an interest in evaluating the success of policies put in place to reduce the health impacts of climate change.
Subject Matter Experts
Marie O’Neill (she/her/hers) has a B.A. from Brown University, an MS in Environmental Health Sciences from Harvard University, and a PhD in Epidemiology from University of North Carolina at Chapel Hill. She has worked for the U.S. Environmental Protection Agency, the Pan American Health Organization, and in Mexico at the National Institute of Public Health and the National Center for Environmental Health as a Fulbright Scholar. Her research interests include health effects of air pollution, temperature extremes and climate change (mortality, asthma, hospital admissions, birth outcomes and cardiovascular endpoints); environmental exposure assessment; and socio-economic influences on health. She served on the Federal Advisory Committee to the third National Climate Assessment. She is a Professor in the Departments of Epidemiology and Environmental Health Sciences at University of Michigan School of Public Health and serves as Faculty Co-Lead for Diversity Equity and Inclusion at the School. She has been involved in several Federally funded research projects that address social disparities in climate effects on health, including a community-based participatory research project based in Detroit called Climate Hazards, Housing and Health.
Kathy Baughman McLeod leads the Center’s global strategy to reach one billion people worldwide with climate resilience solutions by 2030, with a special focus on society’s most vulnerable. She also chairs the Extreme Heat Resilience Alliance (EHRA), a global alliance of 40+ government officials, disaster relief organizations, climate scientists, public health and medical experts, businesses, and nonprofits, that is delivering early warning, policy, finance, and on-the-ground solutions, including appointing Chief Heat Officers in cities around the world. Additionally, she is spearheading the global push to name and categorize heat waves to save lives and build the culture of awareness and preparedness necessary to combat extreme heat. Kathy is currently a member of the World Economic Forum’s Global Commission on “BiodiverCities by 2030” and a member of the Operating Committee of the Insurance Development Forum (IDF). Under her direction, Arsht-Rock is also a managing partner for the UN’s “Race to Resilience” campaign and Resilience Hub at COP26 — the UN’s flagship climate conference. Formerly, she served as Global Executive for Environmental and Social Risk at Bank of America, Managing Director for Climate Resilience at The Nature Conservancy — where she helped devise the world’s first insurance product on a natural asset; a 40 km stretch of the Mesoamerican reef in Mexico. She also served as Deputy Chief of Staff for the elected Treasurer/CFO of the State of Florida, where she was instrumental in making the Florida Treasury the first in the nation to publicly analyze and disclose the financial risks of climate. Kathy was also an appointed Florida Climate and Energy Commissioner. Baughman McLeod is the recipient of the Fuqua School of Business 2021 “Leader of Consequence” award and was appointed to the US Federal Emergency Management Agency’s National Advisory Council as its first-ever climate specialist in 2021. She holds an MBA from Duke University’s Fuqua School of Business and an MS in Geography from Florida State University.
Dr. Harlan’s research explores the human impacts of climate change that are dependent upon people’s positions in social hierarchies, places in built environments of unequal quality, and policies that improve or impede human adaptive capabilities. Focusing on excessive heat and urban water systems as significant and increasingly critical threats to human health and well-being in cities, she studies social systems and landscapes that produce unequal risks for people in neighborhoods divided by social class and race/ethnicity. She has led multi-institutional, interdisciplinary research and community engagement projects that integrate social theories about the historical production of environmental injustices with data and models from the ecological, geospatial, and health sciences. She is currently conducting research on vulnerability to electrical grid failures and water affordability and accessibility in environmental justice communities across selected cities in the United States. Her coupled natural and human systems research has been supported by grants from the National Science Foundation on urban vulnerability to climate change, sustainability and water, the Central Arizona–Phoenix Long-Term Ecological Research program, and national and metropolitan area surveys on environmental attitudes and behaviors. She has served as an advisor on climate justice and social vulnerability to organizations such as the American Sociological Association, the National Center for Atmospheric Research, the US Environmental Protection Agency, and the Social Science Coordinating Committee of the U.S. Global Climate Change Research Program.
Roseann Bongiovanni has worked for environmental justice for more than 25 years. Her extensive career began as a young organizer with the Chelsea Green Space Committee and included victories defeating the construction of a diesel power plant, and preventing ethanol “bomb” trains from traveling to a Chelsea Creek oil terminal. In 2016, Roseann transitioned this vital work into the independent environmental justice and public health organization, GreenRoots, which played a critical role in the response to COVID-19 in Chelsea and East Boston. Under her leadership, Chelsea was named a Culture of Health Prize Winner in 2017, GreenRoots was selected as a Social Innovator in 2018, and was named a US EPA Merit Award Winner in 2021. Roseann has raised and managed millions of dollars for major projects including Creekside Commons Park; federally funded air emissions reduction work, five urban growing spaces; murals and other public art projects; massive tree plantings; and multiple community parks. Roseann has received numerous awards for her work, including the Alternatives for Community and Environment Founders’ Award in 2001, the National Oceanic and Atmospheric Administration Environmental Hero Award in 2006 and the All Chelsea Award “Adult Resident of the Year” in 2007, an MLK Jr. Community Spirit Award by People’s AME Church in Chelsea in 2020 and a US EPA Merit Award in 2021. She has co-authored several publications. Roseann is a lifelong Chelsea resident, a former City Councilor, and City Council President. She has a Masters of Public Health from Boston University and is the mother of two strong-minded children.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.

Climate and Health: What can we do today? Session III
How can data from both the micro (neighborhood and community) level and the macro (national, global) level be used effectively to inform and motivate policy change?


Register
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Friday, March 18th, 2022 12:00 PM – 1:00 PM EST
- Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_CH3.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Leadership and Systems Thinking
- Learning Level: Awareness
- Companion Trainings: Climate and Health: What can we do today? Session I Climate and Health: What can we do today? Session II
- Supplemental materials:None
- Pre-requisites: None
About this Recording
Recent heat waves, wildfires, hurricanes, and other extreme weather events around the world underscore that climate change represents a clear and present danger. Communities everywhere need to better prepare for the extreme weather events we are experiencing today. But how does a community do this?
What you'll learn
At the end of the recording, participants will be able to:
- Describe the creation of large national data platforms by combining health data, socioeconomic data, and climate change-related exposure data
- Discuss the methodological issues in assessing the impact of climate-change exposures and health using large heterogeneous sources of data
- Discuss evidence of climate change-related exposures and adverse health effects from 3 recent epidemiological studies using large national data sets
Moderator

Patrick Kinney
@PATRICKKINNEY20
Professor, Environmental Health, Boston University School of Public Health

@FRANCESCADOMIN8
Clarence James Gamble Professor of Biostatistics, Population and Data Science Initiative, Harvard T.H. Chan School of Public Health
Dr. Kinney joined the School of Public Health faculty in January 2017 as the inaugural Beverly Brown Professor of Urban Health. He was trained as an air pollution epidemiologist at Harvard School of Public Health, and came to BU after two decades at the Columbia University Mailman School of Public Health. In his time at Columbia, he showed how warming temperatures make air pollution like urban smog worse, and more harmful to populations. He led the development of an integrated modeling system to predict the air pollution health effects of climate change into the future. Working at the intersection of climate change, health, and policy, Kinney has conducted research from the South Bronx to China to rapidly growing cities throughout Africa. At Columbia, he also created an interdisciplinary research and teaching program examining the potential impacts of climate change on health. At BU, Kinney is developing a new program that focuses on assessing the health benefits of urban climate action plans, via strategies to promote active transport, green infrastructure, and clean vehicles.
Subject Matter Expert
Francesca Dominici, PhD is the co-Director of the Harvard Data Science Initiative, at the Harvard University and the Clarence James Gamble Professor of Biostatistics, Population and Data Science at the Harvard T.H. Chan School of Public Health. She is an elected member of the National Academy of Medicine and of the International Society of Mathematical Statistics. She is an expert in causal inference, machine learning, Bayesian statistics. She leads an interdisciplinary group of scientists with the ultimate goal of addressing important questions in environmental health science, climate change, and biomedical science. Her productivity and contributions to the field have been remarkable. Dominici has provided the scientific community and policy makers with robust evidence on the adverse health effects of air pollution, noise pollution, and climate change. Her studies have directly and routinely impacted air quality policy. Dominici has published more than 220 peer-reviewed publications and was recognized in Thomson Reuter’s 2019 list of the most highly cited researchers–ranking in the top 1% of cited scientists in her field. Her work has been covered by the New York Times, Los Angeles Times, BBC, the Guardian, CNN, and NPR. In April 2020 she has been awarded the Karl E. Peace Award for Outstanding Statistical Contributions for the Betterment of Society by the American Statistical Association. Dominici is an advocate for the career advancement of women faculty. Her work on the Johns Hopkins University Committee on the Status of Women earned her the campus Diversity Recognition Award in 2009. At the T.H. Chan School of Public Health, she has led the Committee for the Advancement of Women Faculty.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.

Coronavirus Seminar Series: Mental Health in a Time of Crisis
We know that trauma can shape health in the near and long term. How can we mitigate the population mental health consequences of COVID-19?


Register
Course Information
- Audience: Public health professionals, health professionals, community health workers, public interested in the intersection of coronavirus pandemic and mental health
- Format: Webinar
- Date/Time: Thursday, March 26, 2020 4:00-5:00pm ET
- Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hour. Maximum advanced-level continuing education contact hour is 1. Provider ID: SS1131337 Event ID: 03262020.
If you are not seeking CHES/MCHES contact hours, if you complete the evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course. - Competencies: Community
Partnership Skills
- Learning Level: Awareness
- Companion Trainings: Coronavirus Seminar Series by BUSPH
Building the Public Health System of the Future
- Supplemental materials: NA
- Pre-requisites: None
About this Seminar
This seminar explores population mental health in the context of COVID-19. We know that the pandemic is an extreme stressor, and has multiple characteristics that are toxic to mental health.
Note: This seminar was developed and recorded by BUSPH. The BUSPH Coronavirus Seminar Series addresses different aspects of the coronavirus pandemic, bringing together experts to discuss the causes and consequences of this global pandemic. The seminars aim to provide our community and the public with state-of-the-science information about the pandemic and its intersection with public health and keep us all connected to one another during this time.
NEPHTC is making this recording available to the public health workforce with CHES credits and a certificate of completion.
What you'll learn
At the end of the course, participants will be able to:
- Name 4 characteristics that make the COVID-19 pandemic toxic to mental health
- Describe 2 examples of negative mental health impact from past pandemics
- Describe 5 characteristics of a concerted mental health effort during and following the pandemic
- Name 5 empirically-supported elements that are help people adapt in ongoing threat situations
Moderator

Sandro Galea, MD, DrPH
Dean and Robert A. Knox Professor
Boston University School of Public Health
Sandro Galea, a physician, epidemiologist, and author, is dean and Robert A. Knox Professor at Boston University School of Public Health. He previously held academic and leadership positions at Columbia University, the University of Michigan, and the New York Academy of Medicine. He has published extensively in the peer-reviewed literature, and is a regular contributor to a range of public media, about the social causes of health, mental health, and the consequences of trauma. He has been listed as one of the most widely cited scholars in the social sciences. He is chair of the board of the Association of Schools and Programs of Public Health and past president of the Society for Epidemiologic Research and of the Interdisciplinary Association for Population Health Science. He is an elected member of the National Academy of Medicine. Galea has received several lifetime achievement awards. Galea holds a medical degree from the University of Toronto, graduate degrees from Harvard University and Columbia University, and an honorary doctorate from the University of Glasgow.
Subject Matter Experts

Karestan Koenen, PhD
Professor of Psychiatric Epidemiology
Harvard T.H. Chan School of Public Health
Sarah Lowe, PhD
Assistant Professor, Social and Behavioral Sciences
Yale School of Public Health
Patricia Watson, PhD
Assistant Professor, Psychiatry
Dartmouth Geisel School of Medicine
Karestan C. Koenen, PhD aims to reduce the population burden of mental disorders through research, training, and advocacy. She is passionate about using science to overcome violence and trauma, which are major preventable causes of health
problems globally.
Dr. Koenen’s research focus is three-fold. First, she studies why some people develop PTSD and related mental and physical health problems and why some people are resilient when exposed to similar traumatic events.
Dr. Koenen is a co-principal investigator on the NIMH-funded AURORA study, led by Dr. Samuel McLean with Drs. Ronald Kessler and Kerry Ressler. Dr. Koenen also co-leads the PTSD working group of the Psychiatric Genomics Consortium, which
aims to identify genetic variants that increase risk and resilience following trauma exposure. Second, she investigates how violence, trauma, and PTSD alter long-term physical health and accelerate aging. Much of this work is done in collaboration
with the Nurses’ Health Study. Third, she aims to expand access to evidence-based mental health treatment for survivors of violence and trauma. To this end, she co-wrote the book, Treating Survivors of Childhood Abuse: Psychotherapy for
the Interrupted Life with Drs. Marylene Cloitre and Lisa Cohen.
Dr. Koenen leads the NIMH-funded Training Program in Psychiatric Epidemiology and Biostatistics (T32) and the Interdisciplinary Concentration in Population Mental Health.
She also advises masters and doctoral degree students in the Departments of Epidemiology and Social Behavioral Sciences. In addition, Dr. Koenen leads the Trauma Epidemiology and Population Mental Health Research Group for her students
and post-doctoral fellows. The group is primarily a forum for trainees and junior investigators to present and receive feedback on work-in-progress, but also includes presentations on advanced research methodology and career development.
Dr.
Koenen advocates for survivors of violence and trauma. In May 2011, Dr. Koenen testified before the House Foreign Affairs Full Committee about the epidemic of sexual violence and victim blaming culture of the Peace Corps. She has written
for the Boston Globe, the Washington Post, the Huffington Post, and the Women’s Media Center’s Women Under Siege Project, which investigates how rape and other forms of sexualized violence are used as tools in conflict. Dr. Koenen also
consulted on the documentary, It Happened Here, which examined the epidemic of sexual assault on university campuses. In addition, Dr. Koenen speaks to lay audiences about the latest scientific findings around violence and trauma.
Sarah Lowe, Ph.D., is a licensed clinical psychologist and Assistant Professor in the Department of Social and Behavioral Sciences at Yale School of Public Health. Her research focuses on the long-term mental health consequences of a range of potentially traumatic events, as well as the impact of such events on other domains of functioning, such as physical health, social relationships, and economic wellbeing. Her work explores the mechanisms leading from trauma exposure to symptoms, and the role of factors at various ecological levels—from genetics to neighborhoods—in shaping risk and resilience. She uses a range of methodologies to achieve her research aims, including structural equation modeling, latent growth curve analysis, geospatial modeling, and qualitative analysis, among others. Dr. Lowe received her Ph.D. from the University of Massachusetts Boston and completed a postdoctoral fellowship in the Psychiatric Epidemiology Training program at Columbia University Mailman School of Public Health. She previously held an appointment in the Department of Psychology at Montclair State University, where she played a key role in developing the department’s first doctoral program.
Patricia Watson, PhD is a senior educational specialist for the National Center for PTSD and assistant professor at the Geisel School of Medicine at Dartmouth, in the Department of Psychiatry. She is co-author of the Psychological First Aid (PFA) Field Guide and the Skills for Psychological Recovery (SPR) Manual, produced by the National Center for PTSD and the National Child Traumatic Stress Network. She is also a co-author of the Combat Operational Stress First Aid (COSFA) Field Guide, produced by the Department of Defense, the Defense Centers for Excellence, and the National Center for PTSD, and the Stress First Aid and Curbside Manner manuals for fire and rescue personnel, produced by the National Fallen Firefighters Foundation. She has additionally co-edited three books on disaster behavioral health interventions, numerous articles on resilience and early intervention, SAMHSA guidance documents, and articles and chapters on disaster mental health, resilience, combat and operational stress, and pandemic flu.
Registration
Select the Enroll Me button below to register for this webinar. If you have any trouble accessing the webinar, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
* Yale School of Public Health, Office of Public Health Practice, a New England Public Health Training Center partner, is a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. All CHES credit inquiries are managed by YSPH

Encouraging Voter Turnout Ahead of the National Election
How can we promote voter engagement?


Register
Course Information
- Audience: Public Health Professionals
- Format: Recorded Webinar
- Date/Time: Monday, October 17, 2022, 2:00 PM – 3:00 PM ET
- Price: Free
- Length: 1 hour
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hours. Maximum advanced-level continuing education contact hours are 0. Provider ID: 1131137 Event ID: SS1131137_EVTANE.If you are not seeking a CHES/MCHES contact hours, if you complete the post-test and evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Communication Skills
- Learning Level: Awareness
- Companion Trainings: None
- Supplemental materials:None
- Pre-requisites: None
About this Recording
The health of populations is shaped by politics and policies that create the world around us. Elections have real consequences for public health, making voting a central pillar of our community efforts towards creating a better, healthier world. America is Calling. Vote! is an effort to encourage voters under 35 to vote in the upcoming midterm elections. Join us for a conversation between BUSPH Board Member John Rosenthal and March for Our Lives leader David Hogg on the importance of voting and the responsibility of public health to promote voter engagement.
What you'll learn
At the end of the recording, participants will be able to:
- Describe the mission and importance of the effort, America is Calling. Vote!
- Discuss the impact that young voters can have on democracy and freedom in the U.S.
- Discuss the correlation between voter turnout and positive change in past elections.
- Recommend strategies for discussing politics with people who have opposing views.
Moderator

Craig Andrade
@DRCRAIGANDRADE
Associate Dean for Practice, Boston University School of Public Health
John Rosenthal
@JOHNROSENTHAL_
Founder, Stop Handgun Violence; President, Meredith Management
David Hogg
@DAVIDHOGG11
Co-founder,
March for our Lives
Craig Andrade is Associate Dean of Practice and Director of the Activist Lab at Boston University’s School of Public Health (SPH) where he is serves to catalyze and encourage SPH’s public health practice portfolio locally and globally among all members of the school community, including faculty, staff, students, alumni, and community partners. He is also a member of the Dean’s Cabinet and the Governing Council and chairs the school’s permanent practice committee. Previously Dr. Andrade was the Director of the Bureau of Family Health & Nutrition (BFHN) at the Massachusetts Department of Public Health (DPH). BFHN’s programs include Early Intervention (EI), Pregnancy, Infancy and Early Childhood, Children and Youth with Special Health Needs, Women, Infants and Children (WIC) Nutrition Program, Home Visiting, Title V Maternal and Child Health Block Grant, Breastfeeding Initiative, Birth Defects Surveillance, Universal Newborn Hearing Screening Program, the Office of Data Translation and Birth Defects Research and Prevention. He also served as Director of the Division of Health Access at DPH, helped found the Racial Equity Leadership Team and Cross-Department Racial Equity Collaborative at DPH and was Associate Dean of Health and Wellness and Director of Student Health Services at Wheaton College in Norton, MA. He served as critical care, public health and ward nurse at Boston Medical Center; nurse manager and head athletic trainer at Buckingham Browne & Nichols School in Cambridge, MA; and was owner/operator of Active Health, a private health and fitness company. Craig is a registered nurse, athletic trainer, licensed massage therapist and strength and condition specialist with masters and doctoral degrees in public health from Boston University. His research interests include behavioral risk management and resilience-building among children, adolescents and young adults.
Subject Matter Experts
John Rosenthal is the President of Meredith Management. He is a successful real estate developer and manager in Massachusetts who has distinguished himself in his ability to balance corporate and individual responsibility. John is also very active in community based environmental and renewable energy issues as well as social and economic justice. He has organized and advocated extensively in support of safe and renewable energy and against nuclear power and weapons. In February 2022, John partnered with world renowned branding and creative designer, Bruce Mau, and the Massive Change Network to create the America is Calling – VOTE! initiative to rebrand democracy and freedom in America by countering the voter suppression efforts and motivating Americans to vote to help save Democracy.
Thrust into the world of activism by the largest school shooting in American history, Parkland survivor David Hogg has become one of the most compelling voices of his generation. His call to “get over politics and get something done” challenges Americans to stand up, speak out and work to elect morally just leaders, regardless of party affiliation. Passionate in his advocacy to end gun violence, David’s mission of increasing voter participation, civic engagement and activism embraces a range of issues.
Registration
Select the Enroll Me button below to register for this recording. If you have any trouble accessing the recording, contact support@nephtc.org.
Acknowledgement: This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) as part of award 2 UB6HP31685‐05‐00 “Public Health Training Centers.” The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS or the U.S. Government.

Epidemiology and Race: Why and How We Study Racial Health Disparities (Part 1)
How can theory and history help us identify pathways that contribute to racial health disparities in the United States?


Register
Course Information
- Audience: Program administrators/managers, data managers, data analysts and program evaluators, and public health workforce members.
- Format: Webinar
- Date/Time: Thursday, February 25, 2021, 4:30 – 6:00 PM
- Price: Free
- Length: 3 part series, 1.5 hours each
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hour. Maximum advanced-level continuing education contact hour is 1. Provider ID: 1131137, Event ID: SS1131137_ER1.
If you are not seeking CHES/MCHES contact hours, if you complete the evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course. - Competencies: Health Equity Skills
- Learning Level: Awareness
- Companion Trainings:
- Supplemental materials: NA
- Pre-requisites: None
About this Seminar
This series of panels will examine how race and racial health disparities are studied in epidemiology. The first panel in our series will explore the history of census data, how data on race are collected and studied, and the implications of how this data are used in population health science.
What you'll learn
At the end of the course, participants will be able to:
- List six structural or social determinants of health that disproportionately affect persons of color
- Describe relationship of self-identification and social identification of race with health outcomes
- Discuss the importance of understanding causal mechanisms in addressing race and racism in epidemiologic findings
- Discuss the reasons for and the ramifications of limitations of data sets in assessing race
- Discuss the fundamental social causes of health inequalities and how they lead to socioeconomic and racial disparities
- Discuss possible sources of bias that may influence findings about the effects of race on health outcomes
Moderator

Jay Kaufman
President, Society for Epidemiologic Research
Subject Matter Experts

Wayne Giles
Dean and Professor, University of Illinois at Chicago

Chanelle Howe
Associate Professor, Brown University

Jennifer Manly
Professor,
Columbia University

Sherman James
Susan B. King Distinguished Professor Emeritus of Public Policy, Duke Sanford School of Public Policy
Registration
Select the Enroll Me button below to register for this webinar. If you have any trouble accessing the webinar, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
* Yale School of Public Health, Office of Public Health Practice, a New England Public Health Training Center partner, is a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. All CHES credit inquiries are managed by YSPH

Epidemiology and Race: Why and How We Study Racial Health Disparities (Part 2)
What are some key aspects of discrimination and oppression that are important to measure when examining the effects of multiple oppressions on marginalized populations?


Register
Course Information
- Audience: Program administrators/managers, data managers, data analysts and program evaluators, and public health workforce members.
- Format: Webinar
- Date/Time: Friday, February 26, 2021, 10:00 – 11:30 AM
- Price: Free
- Length: 3 part series, 1.5 hours each
- Credential(s) eligible for contact hours: Sponsored by New England Public Health Training Center (NEPHTC), a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. This program is designated for Certified Health Education Specialists (CHES) and/or Master Certified Health Education Specialists (MCHES) to receive up to 1 total Category I continuing education contact hour. Maximum advanced-level continuing education contact hour is 1. Provider ID: 1131137, Event ID: SS1131137_ER2.
If you are not seeking CHES/MCHES contact hours, if you complete the evaluation, you will receive a Certificate of Completion. The Certificate will include the length of the course.
- Competencies: Data Analytics and Assessment Skills, Health Equity Skills
- Learning Level: Awareness
- Companion Trainings:
- Supplemental materials: NA
- Pre-requisites: None
About this Seminar
This series of panels will examine how race and racial health disparities are studied in epidemiology. The first panel in our series will explore the history of census data, how data on race are collected and studied, and the implications of how this
data are used in population health science.
What you'll learn
At the end of the course, participants will be able to:
- Describe how use of race correction in measurement tools may result in inappropriate or invalid interpretation
- Discuss opportunities for addressing implicit bias in using epidemiologic data
- Describe a community intervention to improve medication usage identified by pharmaco-epidemiologic studies
- Explain the difference in the definitions of race based on biology and social constructs and how they relate to disease risk
- Discuss how the concept of “intersectionality” helps understand the effects of racism and oppression on individual, interpersonal, institutional, and structural levels
Moderator

Jay Kaufman
MODERATOR President, Society for Epidemiologic Research
Moderator

Jay Kaufman
President, Society for Epidemiologic Research
Subject Matter Experts

Wayne Giles
Dean and Professor, University of Illinois at Chicago

Chanelle Howe
Associate Professor, Brown University

Jennifer Manly
Professor,
Columbia University

Sherman James
Susan B. King Distinguished Professor Emeritus of Public Policy, Duke Sanford School of Public Policy
Registration
Select the Enroll Me button below to register for this webinar. If you have any trouble accessing the webinar, contact support@nephtc.org.
Acknowledgement: This project is/was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UB6HP31685 “Regional Public Health Training Center Program.” This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
* Yale School of Public Health, Office of Public Health Practice, a New England Public Health Training Center partner, is a designated provider of continuing education contact hours (CECH) in health education by the National Commission for Health Education Credentialing, Inc. All CHES credit inquiries are managed by YSPH